Breading
A fun little video for summer.
read moreGuatemala Mission Trip
Friday, March 15, 2013 As Lisa, Prema, and I head to Guatemala, I am excited to be a part of this Christian Dental Mission Trip. As we go out to serve as the body of Christ, it is really a great experience every time I have served in the capacity of giving away dentistry to
read more
Guatemala before and after
Thursday, March 28, 2013 A lot of people think that when you go on a mission trip to Guatemala that you will do nothing but extractions and that the majority of your impact will be on the physical health of patients as you remove a major source of infection and inflammation from their body. We
read more
Before and After: 2011 to 2014 (Extreme Esthetics)
Wednesday, May 14, 2014 When we started this case, the patient came to me stating unequivocally she was not interested in jaw surgery (orthognathic surgery), but she wanted to improve the look of her smile. I explained that if she was willing to do the work that together we could improve her esthetics and her
read more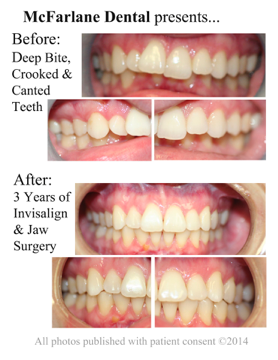
Before and After: 3 Years of Invisalign with Orthognathic Surgery
Thursday, June 26, 2014 We started this case with our eyes wide open. We knew it would require 3 stages: Stage 1: Invisalign to straighten the crooked teeth. Stage 2: Advancement of the lower jaw. Stage 3 below. From the beginning, we knew that this case included a mandibular jaw insufficiency, Class II div 2.
read more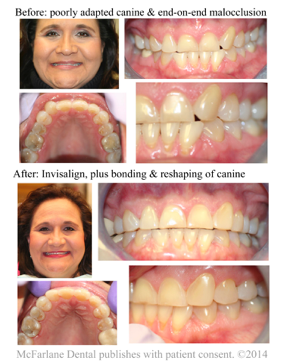
Another beautiful day
A couple of really big dental changes took place for this patient over the past 3 years. I am going to detail the three most significant changes we accomplished with Invisalign, and bonding. I.I corrected end-on-end occlusion to finish the occlusion in mutually-protected occlusion. Before her teeth were end-on-end, leaving her anteriors hitting tip-to-tip, which is
read moreWhy Glass Ionomers? Why now? 2014, (Austin, TX)
McFarlane Dental Announces a New Dental Material McFarlane Dental presents… I am proud to announce that we have added Riva glass ionomer to our offerings of restorative materials. This addition follows the principle of evidence-based dentistry, making decisions based on what research shows is best for patients and long-term outcomes. This material complements our array
read moreAED Automated External Defibrillator
Tuesday, October 21, 2014 Why AEDs? Well, I’m glad you asked. “About 600,000 people die of heart disease in the United States every year–that’s 1 in every 4 deaths.1” When I was in dental school, one of the electives I took was to become a certified teacher of the CPR class. This elective requires you
read moreBest Practices – Sports Mouthguards
Monday, Ferbruary 16, 2015 If you even casually watch NCAA football, NFL football, or high school football, you have probably noticed a significant change in the discussion of concussions. A professionally designed and fabricated sports mouthguard can make a significant difference in the risk of injury. “Because a professionally-made guard is the most comfortable and
read more